Most of us know what it feels like to have an itchy mosquito bite, or to be sneezy and watery-eyed when the pollen count rises or a cat walks into the room. These local immune responses occur when histamine is released from white blood cells, called mast cells. Histamine is also found in many foods, like vinegar, aged cheese, and tomatoes. And some of us can tolerate it better than others — as with pollen or cats.
When the body is unable to break down and process histamine, it results in a systemwide buildup of the chemical, called “histamine intolerance.” According to Amy Myers, MD, who has treated herself for the condition, causes of high histamine levels can include IgE-mediated allergies, gut imbalances like SIBO and leaky gut, a deficiency in the enzyme diamine oxidase (DAO) that breaks down histamine, and the consumption of a lot of histamine-rich foods.
It can also indicate one of two disorders in mast cells themselves, where the cells are overactive or reproduce too quickly.
“Think of your body as a sink and histamine as the water that fills it,” says Greg Plotnikoff, MD, a Minneapolis-based integrative physician and coauthor of Trust Your Gut. “If the drain is completely clogged, it doesn’t take much for the sink to overflow. Or the drain can be wide open, but that won’t matter if you’ve opened a fire hose into the sink.”
Because histamine circulates in the bloodstream and can be found in nearly every human tissue, one person with overload might suffer from intractable headaches, while another could have chronic diarrhea. Other symptoms include hives, wheezing, runny nose, flushed face, headaches, arrhythmia, and low blood pressure. And researchers have found high histamine levels in patients with IBS, Crohn’s, celiac disease, fibromyalgia, and schizophrenia.
While functional physicians like Plotnikoff have begun to recognize that histamine intolerance may play a role in a range of health conditions, it can be tricky to pin down. A typical elimination diet that cuts out gluten, dairy, corn, and soy, the gold standard for detecting food sensitivities, doesn’t always track for histamine issues.
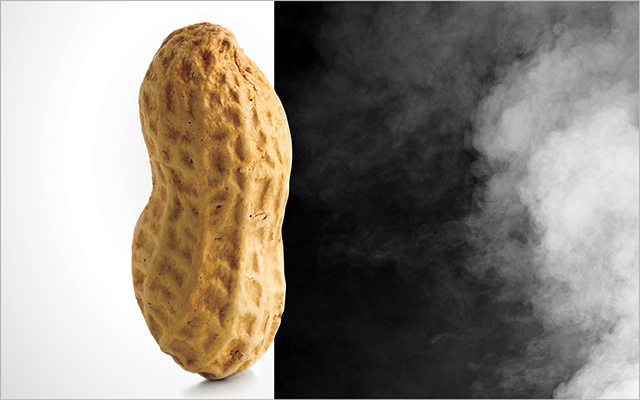
“An elimination diet is designed for patients who need to avoid common food allergens such as milk, egg, or peanut, but it may not address food intolerances. Every patient needs to tailor his or her diet to avoid food allergens and food-inducing intolerances,” says Mariana Castells, MD, director of the Mastocytosis Center at Brigham and Women’s Hospital in Boston.
High-histamine foods are not limited to any food group, although there are a few rules of thumb: Foods that are fermented (wine and vinegar), cured or smoked (charcuterie), produced using yeasts and cultures (bread and yogurt), and aged (hard cheeses) all tend to contain histamine in high concentrations.
“Aged” also applies to leftovers. Many foods that are normally safe — especially meat and fish — may provoke a reaction after they’ve been sitting in the fridge for a few days; histamine levels rise as food begins to break down. Freezing foods eliminates this risk. (See “Foods to Avoid” below for other high-histamine foods.)
If you suspect you may have issues with histamine, what next? Here’s what some functional physicians recommend:
- Investigate all the possibilities.
Start your investigation by eliminating all other possible causes for your symptoms, like more routine food allergies. “If you and everyone you know think you have allergies, but you go to the allergist and all the tests are normal, that’s when you think histamine,” advises Plotnikoff.
For health journalist Yasmina Ykelenstam, who spent 10 years researching histamine issues and became a patient advocate, the first clue she had an issue with histamine came during a fast, when her troubling symptoms disappeared — and returned the moment she resumed eating. “And that’s when I first thought, ‘My God, this has something to do with food.’”
- Track your response to high-histamine foods.
Plotnikoff recommends writing down everything you eat, the timing of your meals, and any symptoms you experience, for at least two weeks. “Many people are surprised,” he notes. “They’ll say I had no idea I ate so many leftovers, or so many tomatoes.”
If a food appears to trigger you, also pay attention to how it was cooked, preserved, stored, and packaged. You may think you’re reacting to a meatball, but you might be reacting to meatball that’s been in the fridge for a few days or sitting in a warming tray all afternoon.
The histamine contained in some raw fruits and vegetables is variable and may be reduced by heating. Also, says Castells, some fruits do not contain histamine but induce histamine release when eaten, and cooking these fruits may eliminate their histamine-releasing properties.
- Know that not all high-histamine foods are created equal, and not every histamine-sensitive person will react to the same foods.
“There can be hundreds or even thousands of types of a certain fruit or vegetable,” Castells explains. “The soil has a tremendous importance in determining the components of each fruit and vegetable and its histamine content, so there could be a tenfold variation in produce grown in California versus South America. How long it takes from the time it’s picked to the time it gets to the table is a factor, and so is how it’s packaged.”
People will have to figure out their own specific triggers and then work around them the best they can. “There isn’t a single gene that we know of that predisposes people to react to histamine,” Castells continues. “There are patients with genetic variations for the enzymes that metabolize and detoxify histamine — such as DAO and histamine N-methyltransferase (HNMT) — but these genetic variations have not been linked to any particular syndrome.”
She does note that a healthy microbiome seems to reduce the strength of histamine reactivity. An intact gut lining prevents foods from “leaking” into the bloodstream and provoking an allergic reaction.
- Try a four-week elimination diet.
If you decide to do trial by elimination, remove high histamine foods and histamine-releasing foods from your diet for a month. (See “Foods to Avoid” below.)
Because freshness plays such a key role, monitor it carefully. Fish that is flash frozen is a better choice than fresh fish from a supermarket, which has often been frozen, thawed, and kept on ice. (Fish and especially shellfish can be a challenge because they deteriorate so rapidly.) Avoid any foods that are highly processed, packaged, boxed, or canned; they often contain preservatives like sulfites that can cause histamine release.
- Keep track of other histamine sources.
Food is not the only source of histamine, and this can confuse your elimination efforts. Seasonal allergies can add histamine to the “sink” in Plotnikoff’s metaphor and may compound your reactions to food.
Cross-reactivity, where the body confuses food with a common allergen, can further complicate matters. “You eat a tomato or a melon and the body mistakes it for your grass allergy,” explains Plotnikoff. Birch allergies are linked to reactivity with several other species — carrot, celery, parsley, apples, cherries, and soybeans among them.
- Develop a sustainable long-term plan.
Castells recommends that her patients stay away from foods that provoke a strong reaction, but she does not recommend a permanent elimination of all histamine-rich foods, because “that kind of diet would be impossible to follow.”
Replace the foods you eliminate for good with foods of equal nutritional value. Ykelenstam counsels people not to become obsessive or afraid of otherwise-healthy foods, like avocados and chickpeas. She does suggest being permanently cautious about inflammatory foods like dairy and wheat.
“The focus should be anti-inflammatory,” she says.
For most people, moderation is the way to go. “With histamine,” Plotnikoff counsels, “dose determines poison.”
Foods to Avoid
If you have a histamine intolerance, try to avoid the following foods, which are rich in histamines, cause histamine release, or block the enzyme that helps the body break down histamine. The following list was adapted from one created by functional physician Amy Myers, MD. You can read more about her histamine protocol here.
- Fermented foods, such as sauerkraut, yogurt, and kombucha
- Vinegar-based foods and salad dressings
- Cured meats like bacon and salami
- Soured foods like sour cream, buttermilk, and sourdough bread
- Dried fruit (because it’s fermented)
- Most citrus fruits
- Wine and beer
- Aged cheese, including goat cheese
- Most nuts
- Avocados, eggplant, spinach, and tomatoes
- All smoked fish and certain species of fish: mackerel, mahi-mahi, tuna, anchovies, sardines
- Bananas, pineapple, papaya, and strawberries
- Chocolate
- Cow’s milk
- Nuts
- Shellfish
- Tomatoes
- Many artificial preservatives and dyes
- Energy drinks
- Black, green, and mate tea



This Post Has 0 Comments