I’ve always enjoyed Maureen Dowd’s sharp-witted, insightful musings in the New York Times, but the only column that sticks in my mind is a piece she penned back in 2014 about sampling a marijuana-laced candy bar in a Denver hotel room.
“I felt a scary shudder go through my body and brain,” she wrote. “I barely made it from the desk to the bed, where I lay curled up in a hallucinatory state for the next eight hours. I was thirsty but couldn’t move to get water. Or even turn off the lights. I was panting and paranoid, sure that when the room-service waiter knocked and I didn’t answer, he’d call the police and have me arrested for being unable to handle my candy.”
In Denver to report on Colorado’s newly legal cannabis market, Dowd learned the next day that the treat she’d purchased from a local pot shop was designed to be cut into 16 pieces and shared — not devoured in one sitting like a Snickers bar. “I reckoned that the fact that I was not a regular marijuana smoker made me more vulnerable, and that I should’ve known better,” she admitted. “But it turns out, five months in, that some kinks need to be ironed out with the intoxicating open bar at the Mile High Club.”
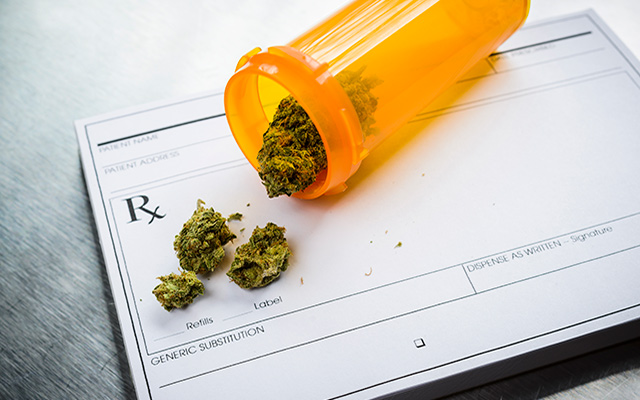
Medical marijuana has since been legalized in several states, including my own, and if recent research is any indication, there are a few kinks the medical-pharmaceutical complex will need to iron out before senior citizens like me — and, I presume, Ms. Dowd — will be seeking a prescription. Like any other pharmaceutical option, cannabis-based medicine (CBM) offers benefits and liabilities. For the elderly, however, the risks may sometimes outweigh the rewards.
It’s been more than 30 years since my last toke, but I’m no more opposed to CBM than I am to prescription drugs in general. That is to say, I’d prefer to avoid pills whenever possible. Still, because CBM has been shown to effectively relieve chronic pain and ease anxiety, I might be more inclined to lean toward that option than a regimen of opioids or other Big Pharma remedies should I encounter such afflictions.
It’s an option older adults are increasingly choosing, notes Massachusetts General Hospital physician Peter Grinspoon, MD. “These patients,” he writes in the Harvard Health blog, “range from people in their 60s with kidney failure who can no longer take certain pain medications but still need to manage chronic pain, to patients in their 90s, who are looking for a good night’s sleep and are leery of the side effects of traditional sleep medications.”
CBMs, however, come with their own side effects, many of which are particularly hazardous for seniors. Grinspoon cites a 2020 review in the Journal of the American College of Cardiology that advises doctors to screen their older patients coping with heart disease before prescribing cannabis. A high dose of CBM could trigger an anxiety attack and coronary distress. And, because older patients tend to take multiple medications daily, the chances of drug interactions increase when adding CBM to the mix.
“Cannabis has about 600 chemicals in it, and in theory, the two main active ingredients in cannabis, THC and CBD, could either increase or decrease the blood levels of other drugs you are taking, by affecting the enzymes in your liver that help metabolize your medications,” Grinspoon explains. Anti-seizure drugs and blood thinners are particularly susceptible to these interactions.
And, as Dowd could probably tell you, it’s all about the dosage. Citing perhaps the most thorough review of what has admittedly been sparse CBM research and its effect on older populations, Donna Fick, PhD, RN, notes in a recent JAMA editorial that researchers found “a significant positive association between THC dose and incidence rate ratio for dizziness or lightheadedness and thinking or perception disorder” among study participants over 50. These side effects can lead to delirium and falls, Fick adds, sending patients to nursing homes and often contributing to a premature death.
“THC should be used with caution in adults aged 50 years and older, and more research is urgently needed to further understand the risks and benefits of THC in adults aged 65 years and older,” she concludes. “THC is prescribed for many conditions where a safer, nondrug approach can and should be used in conjunction with THC or as a safer alternative.”
Dowd survived her cannabis scare, but she left Denver with the distinct impression that neither the state government nor the marijuana industry were much interested in protecting unwitting consumers from similar nightmares. As one retailer told her, “Why should the whole industry suffer just because less than 5 percent of people are having problems with the correct dosing?”
Most physicians, I assume, are slightly less cynical than that pot-shop owner, so I suspect additional research on CBM and its effects on the elderly will eventually lead to safer prescription dosing. And government regulators, I hope, are ensuring that manufacturers are accurately labeling the potency of the products sold in licensed dispensaries.
It’s tempting to believe, after decades of anti-pot propaganda, that a brave new world of medical enlightenment has now dawned. But a drug by any other name is still a drug, and in the hands of a medical system married to pills rather than prevention, CBM becomes just another reason to avoid tending to the root causes of our afflictions.
I should be grateful, I suppose, that there are geezers willing to try CBM. How else will physicians and manufacturers learn about its relative risks and benefits — and, as Dowd so charitably puts it, iron out the kinks? Still, part of me can’t help wondering what these folks have been smoking.



This Post Has 0 Comments