For many women, pain during sex is a problem.
Nearly 75 percent of women report having pain during intercourse at some point in their lives, according to the American College of Obstetricians and Gynecologists (ACOG). For most of these women, pain during intercourse is a temporary problem, but for others, it’s ongoing.
Women can experience pain with sex at any age and for a variety of reasons, from clinical conditions like endometriosis to the decrease in estrogen associated with menopause and the postpartum period. Sometimes, the causes are less self-evident. Take irritable bowel syndrome, for example, which can cause shifts in the pelvic-floor muscles and lead to pain during sex, says Amy Stein, DPT author of Heal Pelvic Pain and coauthor of Beating Endo.
Regardless of the cause, many women wait to seek help — or don’t seek help at all.
“It’s amazing how much women will tolerate before they speak up,” says Barb DePree, MD, OB/GYN, who specializes in sexual health during perimenopause and menopause. “I have patients who will say, ‘Well, I tried this lubricant,’ or ‘I tried a glass of wine to relax,’ but the underlying physiology is what needs to be addressed.”
Even when they seek help, many women don’t get the help they need — at least at first. “When I first started in this field, it took about 15 years to get someone to believe that you had sexual pain,” says Jessica Drummond, DCN, PT, who specializes in pelvic-health conditions. Now, she says, that timeline is down to seven or eight years.
“I can’t tell you the number of patients who haven’t had intercourse for five or six years because their internist said, ‘There’s not much we can do about this,” says DePree. “The women I see in my practice didn’t take no for an answer. It makes me wonder how many women did accept it.”
Pain during intercourse can lead to low (or no) sexual activity, which can contribute to feelings of anxiety and depression, negative body image, relationship problems, and diminished quality of life.
We asked experts to explain some of the top causes of pain during intercourse for women and how to address them:
1. Endometriosis
This painful condition is the result of endometrial-like tissue growing outside the uterus in such places as the fallopian tubes and ovaries. This alone can cause pain with sex, but it can be especially painful if endometrial tissue implants in and around the vaginal canal. “It’s common that endometrial tissue gets stuck in the vaginal area, adheres to the tissue, and doesn’t want to move,” says Stein. “Then imagine having sex. The in-and-out motion is very painful.”
Consult a trusted healthcare provider if endometriosis is interfering with your sex life. But note that some medications prescribed for endometriosis can lower estrogen and cause other problems related to pain during sex. (More on low estrogen and painful sex, below). It can also be worth consulting with a functional-medicine provider, or another trusted holistic practitioner, because lifestyle strategies — like shifts in nutrition — may help ease symptoms of endometriosis when used with other strategies.
2. Vulvodynia or vaginismus
Vulvodynia is marked by chronic pain, burning, or irritation around the vulva that has no identifiable physical cause.
Vaginismus is the spasming of the muscles around the vagina during sex or when inserting a tampon, and it also has no identifiable, physical cause.
If you suspect you have either of these conditions, first ask your doctor to run some tests to exclude other possible diagnoses, like yeast or bacterial infections. Once you’ve ruled out other conditions, work with your doctor to develop a treatment plan, which will vary for each person based on your unique situation. Treatment options for both conditions can include pelvic-floor physical therapy and local anesthetic creams. Biofeedback therapy has shown promise in helping with the symptoms of vulvodynia. Doctors may also recommend other medications for vulvodynia, including anticonvulsants, antidepressants, antihistamines, and nerve block injections.
3. An imbalance of good and bad bacteria in the vagina
Every area of the human body that comes into contact with the external environment has a microbiome. That includes the gut, of course, but also the lungs, skin, eyes, and vagina. When the balance of good and bad bacteria in the vagina gets thrown out of balance, it can lead to itching, irritation, and discomfort during sex. Have your doctor test for bacterial vaginosis or a yeast infection. Antibiotic pills and antibiotic and antifungal creams can be prescribed for vaginal dysbiosis. And like gut dysbiosis, an imbalance of bacteria in the vagina can be helped by lifestyle interventions, including reducing or eliminating sugar from the diet, taking a high-quality probiotic, and staying hydrated.
4. A reaction to perfumed soap or a douche
Soaps with perfumes and synthetic fragrances can irritate the delicate skin in the vulva and cause contact dermatitis. Douches present the same problem, as well as wreaking havoc on the vaginal microbiome. Experts recommend never using a douche (whether you have pain with sex or not) and switching to unfragranced, natural soap.
5. Perimenopause and menopause
Perimenopause is the decade (or more) before menopause when a woman’s reproductive hormones, including estrogen, start shifting in unpredictable ways. Menopause is marked by the end of a woman’s menstrual cycle — around age 51 for most women — and is when estrogen production declines precipitously. Estrogen is the hormone responsible for keeping the walls of the vagina thick, elastic, and lubricated. Without it, the vaginal walls can become thin and less flexible, and vaginal dryness can be a problem.
“You have estrogen receptors everywhere in the body — brain, skin, breasts — but the most concentrated receptors are in the genitals, so over time we see the greatest change in the vulva and vagina during menopause,” says DePree. Vaginal dryness can be addressed by anything that brings blood flow to the vagina, says Mary Jane Minkin, MD, a practicing gynecologist and a clinical professor of obstetrics, gynecology, and reproductive sciences at Yale University.
That includes foreplay, vibrators, and sex itself. “One of our primary treatments for vaginal atrophy is to have sex. It increases blood supply to the area and it is great for the pelvic-floor muscles,” says DePree. “The 70-year-olds who are not being treated for vaginal atrophy are having sex frequently. It is a protective mechanism.”
Vaginal atrophy, which some experts now refer to as the genitourinary syndrome of menopause or GSM, has other safe and effective treatment options. Over-the-counter vaginal moisturizers “work quite well,” says Minkin, who recommends them for ongoing moisturization, and a high-quality lubricant is helpful during sex. Just don’t buy either one in the giant economy size to begin with, cautions Minkin. Different bodies will react to different ingredients, and it might take a few tries to find the best products for you.
If over-the-counter remedies don’t help, talk to your gynecologist about topical vaginal estrogen, vaginal suppositories, and a ring that contains estrogen that is placed in the vagina. “These are very safe medications,” says Minkin. “Only a tiny bit gets absorbed by the body, so you don’t need to worry about blood levels of hormones.” Women with a history of estrogen-receptor positive breast cancer should carefully consider the decision to use topical estrogen (and in conjunction with their oncologist). Data does not show an increased cancer risk for women who have a history of breast cancer who also use vaginal estrogen, according to ACOG, but the organization still advises women who are currently in treatment for breast cancer or who have a history of breast cancer to try non-hormonal remedies first.
6. Hormonal birth control pills (HBC)
Certain medications change the tissue integrity at the vaginal opening, says Stein, and that includes hormonal birth control. The pill fosters a high-progesterone, low-estrogen environment in the body — and, as with perimenopause and menopause, less estrogen is correlated with vaginal dryness, thinner vaginal walls, and less vaginal elasticity. “We have 25-year-old girls who have been on HBC for eight years and their tissue has changed because of birth control,” says Stein. IUDs tend to have less of this effect (though they still can lead to symptoms for some women). If you think HBC might be contributing to pain during intercourse, talk to a licensed healthcare provider about alternative birth-control methods.
7. Estrogen-blocking drugs
Women who have a history of estrogen receptor-positive breast cancer may be prescribed drugs (like Tamoxifen) that block estrogen from being absorbed by the body. Women with endometriosis are sometimes prescribed drugs that block the pituitary gland from stimulating the ovaries to produce estrogen (these drugs are called gonadotropin-releasing hormone agonists or GnRH agonists). These are important treatments for serious conditions, but they can result in the overall lower estrogen that contributes to vaginal atrophy. If you take one of these drugs, consult your oncologist or gynecologist (or both) about strategies for addressing pain during sex.
8. Postpartum period and breastfeeding
Estrogen plummets after giving birth and during breastfeeding and can lead to perimenopause- and menopause-like symptoms. Hormone replacement therapy and local hormone treatment can be considered during the postpartum period. Talk to your OB-GYN about options.
9. Extreme exercise
Extreme exercise can lead to lower estrogen levels, says Drummond. If you suspect overtraining is contributing to symptoms of vaginal atrophy and pain during sex, work to add more rest days into your routine. If intense exercise has become part of your routine and you find it hard to give up (for any reason), consider working with a counselor or therapist to explore your relationship with exercise.
10. IBS or other GI disorders
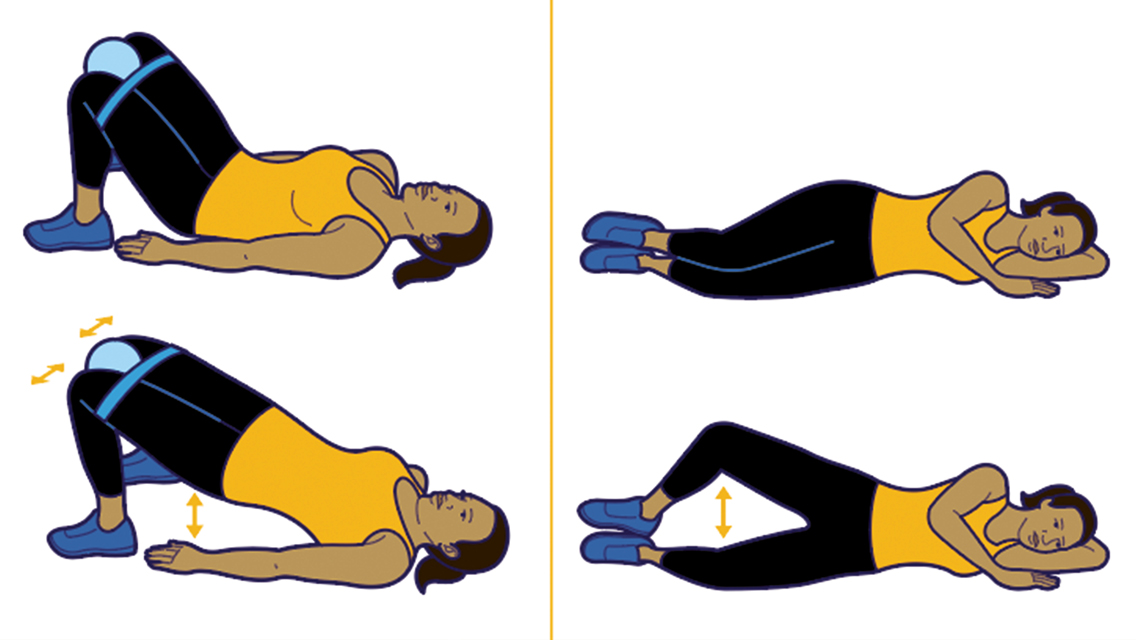
The gut pain that comes along with IBS and other digestive disorders “can cause people to reflexively tighten the whole area, including the pelvic-floor muscles,” says Stein. Same with people who have alternating constipation and diarrhea: They may reflexively tense and strain all the local muscles when their gut is giving them trouble. Pelvic-floor physical therapy can be a tremendous help when the cause of pain during sex is muscular or skeletal.
11. Lower-back pain
As with GI pain, lower-back pain can cause sufferers to reflexively tense all the muscles in the lower part of their torso, including the pelvic-floor muscles, and that can lead to pain during sex. Again, a pelvic-floor physical therapist can help address painful sex when the cause is musculoskeletal.
12. Pelvic or abdominal surgery
Scar tissue can build up after a pelvic or abdominal surgery and contribute to pain during sex. Any surgery can cause this for any woman, but it is especially common for transgender women who have had gender-confirmation surgery. “A lot of trans women will get vaginal-canal surgery and it is not deep enough or wide enough and that is where physical therapy can be helpful, by working with scar tissue and trigger points,” says Stein.
13. Clitoral pain
This can be caused by nerve damage from a new or old injury, say hitting the crossbar of a bike on a recent ride or when you were a kid. Physical therapy can help with clitoral pain if the musculoskeletal system is involved (as it often is with injuries). Women with clitoral pain should also consult with their gynecologist or other trusted healthcare provider.
14. History of abuse
“Pain during intercourse is NOT all in one’s head,” Drummond emphasizes. “But childhood trauma can make the brain more vulnerable to sending a pain signal, even if there is no identifiable tissue damage.” Pelvic-floor physical therapy can help patients with a history of sexual trauma. “We train patients to relax those muscles again,” says Stein. “There are limitations for sure, but we can often help them reduce tightness and muscle spasms.” It’s important for anyone with a history of sexual trauma to work on the emotional aspects of their pain, too. Working with a good therapist can be a key part of healing emotional and sexual trauma.



This Post Has 0 Comments