Explore this article:
It’s that time again. Flu season is upon us, and everywhere we turn — from the family doctor’s office to the nightly news — we are reminded to get our flu shot.
It couldn’t be easier: You can get an influenza vaccine at your favorite neighborhood pharmacy, right along with your toothpaste and shampoo, or at a makeshift stand at the grocery store. At more and more businesses, employees can get one just down the hall from their desks.
During the 2010–2011 influenza season, about half of all children and 41 percent of American adults received flu shots. And health officials are pushing for more. The Centers for Disease Control and Prevention (CDC) “recommends that everyone 6 months of age and older get the annual flu vaccine,” says Joseph Bresee, MD, chief of the Epidemiology Prevention Branch at the CDC’s Influenza Division.
Not all experts agree with this advice, though. An increasing number of researchers, academics and doctors are questioning the scientific basis for an influenza vaccine at all. Some point out that the influenza virus isn’t the cause of most flu-like illness, diminishing the advantage that widespread vaccination confers. Others argue that flu shots don’t work well for the most vulnerable among us, including the elderly, because their immune systems are too weak to respond. The most vocal critics even point to studies showing the influenza vaccine is no better than a placebo.
There’s also a safety concern, since many influenza vaccinations contain toxins such as thimerosal, a preservative containing mercury that was removed from most (but not all) children’s vaccines more than a decade ago.
The rising furor over the influenza vaccine differs from the controversy over most other vaccines because the central argument is not over the risk but rather if it works at all. Defenders insist that widespread vaccination will confer a herd immunity to the general population, protecting the weakest among us, who might actually succumb to influenza if exposed. They say that manufacturing an influenza vaccine year after year keeps the factories primed for the dreaded day a more virulent strain threatens a true pandemic, like the one that killed hundreds of thousands of Americans in 1918. But skeptics label such benefits hypothetical at best, and argue that even the smallest risk or side effect is unacceptable.
Origins of Influenza
No one knows for sure when influenza began circulating through human populations, but since highly transmissible viruses require densely inhabited areas to spread, most medical historians trace the disease to the establishment of cities.
The first description of what sounds like influenza comes from the ancient Greek philosopher and physician Hippocrates. Reports of the rapid spread of fever, body aches and respiratory distress were issued regularly in the densely packed Greco-Roman world.
The most severe influenza pandemic to date hit in 1918 and swept the globe for two years, infecting about 30 percent of the human population and killing an estimated 40 to 50 million people (675,000 in the United States alone).
When influenza kills, the most common victims are young children, the elderly and people with compromised immune systems. The great 1918 pandemic was unusual because it claimed the lives of so many healthy young adults. The fierce pathogen was no ordinary influenza strain — it was avian; as a bird flu, it was particularly foreign to the human immune system — which most likely explains the bizarre mortality pattern.
By the 1940s, researchers had classified influenza into multiple types — A, B and C — based on their protein compositions. Eventually, they subdivided these types further, based on external structure, which determines how a particular virus invades and colonizes the human respiratory system.
One category of shell protein, called hemagglutinin (H), is characterized by spiked extensions that spearhead the initial invasion. Another category, called neurminidase (N), helps viral particles capture new terrain once invasion has occurred.
Thus far, three types of H and two types of N have been associated with widespread human infection, giving influenza its dreaded alphanumeric acronyms. H1N1, for instance, is a type-A swine flu that made a landing in 2009.
The increasingly ubiquitous H3N2, another type-A virus that infects humans, pigs and birds, was isolated in the United States as recently as last year.
Chasing Data
When the influenza pandemics of 1957 and 1968 hit, scientists were able to identify the diseases’ predominant viral strains and design preventive vaccines tailored to those strains.
The problem, even back then, was that there were several variations of influenza strains circulating the globe, says medical historian George Dehner, PhD, author of Influenza: A Century of Science and Public Health Response. The variants of those strains mutated constantly, far too quickly for the vaccines to keep pace.
Over the years, with the advent of new DNA sequencing technologies, scientists have become better at rapidly isolating influenza strains and producing updated vaccines. But it is still an inherently inexact science, unable to keep up with the speed at which viruses can spread and morph, a phenomenon dramatically amplified by global travel in recent years.
Meanwhile, the controversy over vaccination has intensified. Some experts question whether flu inoculations are even focused on the right target. Epidemiologist Tom Jefferson, MD, author for the independent Cochrane Acute Respiratory Infections Group, suggests the incidence of influenza is greatly inflated because it is systematically confused with influenza-like illness, a syndrome caused in minor part by influenza viruses, but more frequently attributable to other viral and bacterial agents. “Conflation of influenza with influenza-like illness has confused the situation and fueled a frenzy,” he says.
Experts like Jefferson caution against using the words “flu” and “influenza” interchangeably, noting that “flu” is a more loosely defined category that includes viruses that are not influenza-based, but just happen to cause very similar clinical symptoms.
To illustrate, Jefferson points to Flu Trends (www.google.org/flutrends), a site that estimates flu incidence around the world based on the number of flu-related search queries in each region. “Users of Flu Trends think they are following the spread of influenza,” he notes, “while in reality, the site depicts the spread of influenza-like illness.”
Virologist Kennedy Shortridge, PhD, agrees. “There are a number of infectious agents that can mimic flu,” says Shortridge, a professor emeritus at the University of Hong Kong and a pioneer in studying the origin of influenza. “In many cases, no laboratory diagnosis of influenza is made.”
To find out how many cases of influenza-like illness are actually influenza A or B, scientists would need to take a random sample of people diagnosed with influenza-like illness, and then test them for every possible causal agent and illness. The formal studies are few, but Jefferson has completed calculations based on data from trials for vaccines, and he estimates that, on average, only about 7 percent of those with influenza-like illness actually have influenza.
“The CDC and the media portray influenza as a deadly threat,” he says. “But the data suggest that seasonal influenza is a relatively rare and benign condition, with an incidence not exceeding 1 percent in the general population during autumn and winter months.”
Part of the problem is a lack of evidence for the deaths often attributed to influenza, says Peter Doshi, PhD, a postdoctoral fellow in comparative effectiveness research at Johns Hopkins University School of Medicine in Baltimore. The CDC put the death toll at 36,000 in 2003, though it has recently backed off the claim. “There is no actual body count here, as we have with death by car accident or cancer,” Doshi says. Rather, the numbers are broad estimates, made when the CDC uses statistical modeling to associate “excess deaths” with periods of elevated influenza-virus circulation. “But since there is no guarantee that what they call influenza is actually influenza,” says Doshi, the whole model is unreliable.
Jefferson and his Cochrane team performed a meta-analysis — a study of studies — using the best research data they could find on influenza vaccines. In their subsequent report, published in the British Medical Journal in 2009, they concluded that there was little evidence to support continued widespread use of vaccine for influenza.
On average, says Jefferson, perhaps one adult out of 100 vaccinated will get influenza symptoms compared with two out of 100 in the unvaccinated group.
“After reviewing more than 40 clinical trials, it is clear that the performance of the vaccines in healthy adults is nothing to get excited about,” he says. “Public health interventions such as hygiene measures and barriers to interrupt or reduce the spread of respiratory viruses have a much better evidence base than vaccines. They are also cheaper, yet they are almost ignored.”
An Informed Choice
There are certainly plenty of experts who still endorse the influenza vaccine. One is immunologist Mary Ruebush, PhD, best known for her book, Why Dirt Is Good: 5 Ways to Make Germs Your Friends. “Getting the flu vaccine is like taking your immune system to the gym,” Ruebush says. “Your immune system is activated when it responds to the vaccine, keeping it primed for response when the actual virus hits.”
Ruebush and others believe the best course is for the healthy among us to get vaccinated, not so much to protect ourselves from a bout of influenza, but for the benefit of seniors and others who don’t mount enough of an immune response, regardless of whether or not they are vaccinated. The tactic invests a population with what public health experts refer to as “herd immunity.’”
Still, even in healthy populations, vaccines typically protect against just three or four strains, not the multiple strains that are constantly mutating in the wild. So, even if a vaccine boosts immunity, it can never protect against the full range of a constantly shifting illness.
After weighing the benefits of this marginal level of coverage, you might well decide to skip this year’s trip to the clinic. Then again, you may decide something is better than nothing, and elect to follow the advice of mainstream medicine and the CDC.
If you choose the latter path, there are a few things to keep in mind.
First, the flu vaccine is prepared in hen eggs — so if you are allergic to eggs, you could have a reaction. You should also ask questions about the chemical makeup of your shot. The majority of flu vaccines come in multidose vials preserved with thimerosal, a form of the heavy metal mercury that has been widely implicated in neurological and inflammatory disease. (Single-dose vials and the live flu-vaccine mist are generally thimerosal-free.)
Doshi also wants people to know that flu vaccines are biologics, “meaning they are made with living materials,” he says. “Problems with the manufacturing process continue to crop up,” he notes, because dealing with living material presents challenging complexities, and contamination is a near-constant threat.
He points to the recent spike in cases of narcolepsy in Finland and febrile convulsions in Australia in 2009 following vaccination. Use of the respective vaccines was discontinued and the problems disappeared, though the root causes were never determined. “The process is messy,” and it’s impossible for something retooled each year to be risk-free.
Jefferson also points out that advisers on government vaccine committees vested with product approval have suspect ties to the manufacturers. With many of pharma’s most profitable drugs coming off patent in recent years, new vaccines, including influenza vaccines, have taken on an added luster. Experts predict that the seasonal influenza-vaccine market will grow to a $4 billion a year industry by 2015.
Despite all this, Doshi believes that a concern for the public’s well-being is what motivates most health officials. Looming in the back of everyone’s mind, after all, is the fear of another great pandemic. Pharmaceutical companies have convincingly argued that we must maintain a “growing and stable” market for garden-variety annual influenza vaccines. Otherwise, they warn, when the next flu pandemic hits, we won’t have mechanisms in place to stay ahead of the disaster — and we’ll be defenseless in its wake.
Jefferson doesn’t buy this argument: “Vaccine policies are made on the basis of personal belief. Once the policies are made, those who made them [selectively] publish the evidence to support their point of view. They keep justifying their policy on the basis of studies done by pharmaceutical companies, and they are unwilling to reexamine their decisions and reevaluate the policies.”
Shortridge points out another problem. “When a pandemic virus emerges,” he says, “it takes time for the world to recognize that it is on the cusp of a pandemic. Time for preparation of a vaccine and safety testing hinder widespread distribution and protection.”
Meanwhile, the World Health Organization and the CDC continue to push for widespread influenza vaccination as the most effective means of prevention, and many experts flat-out reject the notion that influenza is benign.
This debate will likely rage for years. So for now, each of us is left to make up our own mind about whether to get that shot — or not.
Natural Ways to Prevent Getting the Flu
Whether or not you choose to get a flu shot, many experts stress that simple, commonsense measures are the best way to prevent most strains of the flu. Here are some basics to consider embracing:
- Avoid close contact with sick people whenever possible.
- When you are ill, stay home from work, school and errands in consideration for others. Urge your friends, family and coworkers to do the same.
- During flu season, wash your hands frequently to protect yourself and others from germs.
- Cover your mouth and nose with a tissue when coughing or sneezing.
- Keep your hands away from your face. Germs routinely spread when a person touches something contaminated with germs and then touches his or her eyes, nose, or mouth.
- Stick to a nutrient-dense, toxin-free diet, and avoid foods that tend to weaken the immune system, such as sugar, refined grains, industrial vegetable oils, and processed and refined foods.
- Support your immune system by getting plenty of sleep and avoiding chronic stress. Constant anxiety at work or in your relationships suppresses the immune system, opening the door to flu.
- Get plenty of sunshine and supplemental vitamin D. High levels of vitamin D have long been linked to lower rates of flu.
- Get at least 20 minutes of exercise a day to prime the immune system. (See “Does Exercise Boost the Immune System?”)
- Avoid antibiotics and antibacterial cleansers and sanitizers whenever you can. They can weaken your natural defenses and entice your “immunity muscles” to atrophy. By steering clear of chemical antibacterial agents as much as practical, you’ll encourage your body’s immune system to get smarter and harder-working over time. As a result, it will stand a better chance of effectively vanquishing infections and diseases of all kinds, including influenza.
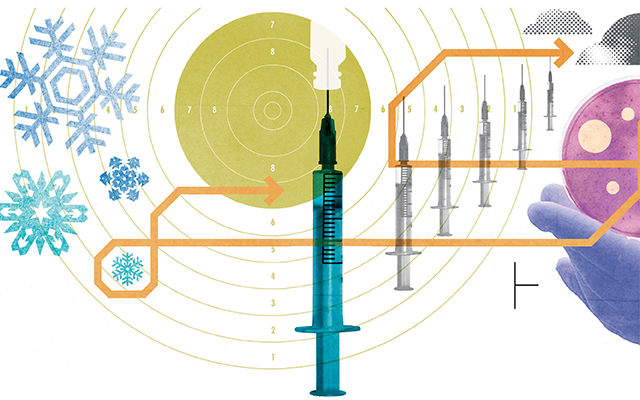
What’s in a Flu Shot?
Pharmaceutical companies manufacture many varieties of influenza vaccine, and formulations change from year to year, along with the targeted strains. To make the vaccine, about six months prior to the next influenza season, scientists identify the strains they believe will be circulating most widely in the next year (generally two As and one B) and inject them into fertilized hen eggs. After the virus multiplies in the eggs, it is harvested, and then weakened for use in live viruses, or inactivated with a chemical such as formaldehyde for injectable killed-virus vaccines.
Finally, the product is purified to elicit an immune response without making the patient sick, and shipped to medical centers and other facilities where patients can receive the vaccine. Killed-virus vaccines are delivered via an injection, which may come from multidose vials — which often contain thimerosal, a toxic preservative — or in single-dose syringes that have far less thimerosal, or none at all. Other times, patients (particularly the very young) inhale live-but-weakened versions of influenza organisms in the form of a mist. These do not contain thimerosal. Here are some of the potentially harmful toxins still found in various influenza vaccines. Make sure to ask your healthcare provider whether they’re in your flu shot.
- Thimerosal is a mercury-based preservative that was removed from other vaccines used in children in 2001.
- Polysorbate 80 is linked to infertility.
- Formaldehyde is classified as a human carcinogen by the Department of Health and Human Services. One version of the flu shot used in the United States uses formaldehyde to inactivate the influenza virus in the vaccine-manufacturing process, after which the formaldehyde is purified out, but trace amounts may remain.
- Octoxinol-10 is commonly used as a vaginal spermicide.
Note: Many people worry that they will be exposed to yet another heavy metal, aluminum, but it is not used in U.S. flu vaccines.



This Post Has 0 Comments