When energy flags, many of us reach for sweet or starchy snacks — a bagel, a mocha latte, a candy bar from the cafeteria vending machine — to help push us through. While these treats might deliver an immediate power surge, the strategy tends to backfire. Just as quickly as our energy spikes, it crashes, leaving us more sluggish than before.
The long-term effects of these foods are worse. It’s true that the body uses carbohydrates and sugars found in whole foods; it converts them to glucose, which is an important source of cellular energy. But diets overloaded with refined sugar paradoxically undermine our ability to generate the energy we need to go about our daily lives.
The sweet stuff hides under a variety of names in many products (including ketchup, coffee creamer, spaghetti sauce, and peanut butter) and refined carbohydrates (think bread, pasta, and cereal).
Observed through an evolutionary lens, our proclivity for sweet, starchy foods makes sense. Sweet-tasting berries and high-carb wild tubers, for instance, were once rare, seasonal finds and important sources of fuel for our ancestors’ bodies and brains.
Unfortunately, sugar is ubiquitous in today’s food supply. It’s also been manipulated to be addictively hypersweet and nutritionally bankrupt. Meanwhile, refined carbohydrates, such as white flour, digest quickly into glucose — and most of us get more processed carbs than we need.
These foods don’t just offer empty calories. They upset the body’s finely calibrated biochemistry, effectively confusing hormones and contributing to metabolic dysfunction — a breakdown in the body’s ability to synthesize energy from food. This makes us decidedly unenergetic after the rush, and it has significant health consequences over time.
Many experts, in fact, maintain that too much dietary sugar and too many processed carbohydrates are the primary forces fueling the global epidemic of metabolic disorders, including obesity and type 2 diabetes. They’ve linked high-sugar diets to a host of debilitating and life-threatening conditions: hypertension and heart disease, Alzheimer’s, cancer, liver disease, hormone-related disorders, and more.
While chronic health conditions are multifactorial, the corrosive nature of sugar and processed carbohydrates cannot be understated. To appreciate their negative impact, it’s helpful to understand the relationship between blood sugar and the hormone insulin.
Insulin Overload
After you eat, your digestive system breaks the carbohydrates in food into glucose molecules, which are then released into your bloodstream. Detecting an increase in blood sugar, your pancreas excretes insulin — a hormone that’s responsible for helping the body metabolize carbohydrates and manage blood sugar. Insulin signals muscle, liver, and fat cells to pull the glucose out of your bloodstream and store it as an energy source.
This postmeal insulin response is an essential physiological process designed to keep blood glucose at healthy levels. A meal low in sugars and refined carbohydrates — an omelet with a side of sautéed greens, for instance — triggers a slow, steady stream of insulin over the next several hours.
Conversely, a meal loaded with sugars and fast-digesting carbohydrates — imagine a stack of pancakes covered in maple syrup and washed down with a glass of orange juice — causes your blood glucose to spike and your pancreas to quickly produce a surge of insulin.
Diets that are regularly high in sugar and refined carbs (think pancakes) keep the insulin response in overdrive. Eventually, your liver and muscle cells start to think your pancreas is crying wolf — and they stop listening to insulin’s signal to let glucose in.
“Insulin is constantly being released by the pancreas, but the cells reject it,” explains nutritionist Dee Harris, RD, LDN, a certified diabetes educator and functional-medicine practitioner. No longer sensitive to insulin, the cells stop responding, and both glucose and insulin return to the bloodstream. This dangerous condition is known as insulin resistance.
A number of other factors can exacerbate insulin resistance: low activity levels (which affect glucose absorption), bacterial imbalances in the gut microbiome, nutrient deficiencies, and exposure to endocrine disruptors in the environment.
High circulating insulin simultaneously blocks weight loss and drives weight gain, setting the stage for chronic health conditions associated with obesity. It obstructs lipase, the enzyme responsible for breaking down fat in the liver. At the same time, it makes it easier for glucose to penetrate fat cells, which remain somewhat sensitive to the hormone even as muscle cells become resistant. Researchers are investigating other mechanisms by which insulin may affect weight and, consequently, broader health.
Insulin’s effect on weight may be -independent of high blood sugar. A 2013 study published in the American Journal of Clinical Nutrition found that high levels of insulin — but not necessarily high blood sugar — predicted weight-loss resistance and the tendency to gain weight in obese individuals.
“Insulin is like Miracle-Gro for your fat cells,” says pediatric endocrinologist David Ludwig, MD, PhD, professor of nutrition at Harvard School of Public Health. “It’s just not the miracle you want in your body.”
Further, diet-intervention studies with human subjects have found that high sugar intake increases the lipids circulating in the bloodstream, contributing to cardiovascular disease.
“Insulin resistance causes changes to the whole biochemistry of lipid metabolism, including elevated triglycerides,” explains Cindi Lockhart, RDN, LDN, IFNCP, senior manager of nutrition education and research for Life Time Medical and Total Health.
“It also reduces levels of protective cholesterol while increasing the kind of cholesterol that damages blood vessels and elevates the risk for heart disease,” she says. (To learn more about the latest thinking on cholesterol and heart health, go to “Rethinking Heart Health“.)
Glucose Stress
Ongoing research suggests that insulin resistance also generates too much circulating glucose, or blood sugar. High glucose levels put stress on the metabolic system, which can result in the formation of harmful compounds called advanced glycation end products (AGEs). Also known as glycotoxins, AGEs can cause cellular damage to the cardiovascular system, kidneys, liver, muscles, and brain.
High blood sugar is also associated with increased levels of free radicals — molecules that damage healthy cells, weaken the immune system, and make the body more hospitable to cancer. In addition, research strongly links it to inflammation, the scourge of most chronic lifestyle conditions, including type 2 diabetes.
Chronically elevated blood sugar has been shown to shrink the hippocampus, the memory center of the brain, causing researchers to connect it with Alzheimer’s disease and other forms of cognitive decline.
“Many practitioners now identify Alzheimer’s as type 3 diabetes,” says Harris, noting a 2013 study published in the New England Journal of Medicine suggesting that diabetics are four times more likely than those without the disease to develop dementia.
Insulin stimulates the production of antioxidants and protects against glycation, explains nutrition scientist Chris Masterjohn, PhD. But when the insulin-response mechanism goes awry, that protective benefit disappears. “Insulin does a lot of things that are good for health. When you lose insulin signaling, you lose all of insulin’s health-promoting qualities.”
Hormone Disruption
Too much insulin in your bloodstream can also disrupt your other hormones, explains Lockhart.
“All of your hormone systems are coordinated through the hypothalamic-pituitary-adrenal-thyroid-gonadal, or HPATG, axis in the body,” she says. Imagine this axis as an intricate and integrated web, and it’s easy to see how a disruption to one hormone system can produce disruptions in other areas.
In addition to signaling cells to take up glucose, insulin influences the sex hormones estrogen and testosterone. Insulin resistance has been associated with polycystic ovarian syndrome and infertility in women, while metabolic syndrome — which is characterized by insulin resistance — is closely linked to testosterone deficiency in men.
Insulin and cortisol affect one another as well, which explains why stress can contribute to insulin resistance. “Anytime you activate the stress response, your body will release cortisol to prepare for fight or flight,” says Lockhart.
The release of cortisol triggers your liver to send glucose into your bloodstream, which can elevate blood sugar and the risk for type 2 diabetes.
Balance Your Blood Sugar
How much your blood glucose and insulin surge after eating sugar and carbohydrates depends on genetics, stress (including physiological stressors like illness and food sensitivities), gut health, your activity level, and your previous meal.
For instance, if you eat a sugary or high-carb breakfast, remain sedentary until noon, and then eat a high-carb lunch, your muscle cells probably don’t need much in the way of fuel; they got plenty at breakfast, and you haven’t moved much since. But the glucose from your lunchtime meal has to go somewhere, so it’s forced into fat cells for storage, contributing to weight gain.
On the other hand, if you didn’t eat for 14 hours overnight and then hit the gym before eating that same breakfast and lunch, your muscles would be running low on fuel and have room to absorb more of the glucose. (Note that fuel-storage space in muscles isn’t limitless; dysregulated blood sugar and insulin can affect endurance athletes as much as couch potatoes.)
Because so many factors influence your body’s response to glucose, it’s helpful to have some strategies for anticipating what sets your blood sugar into orbit and what doesn’t. Try these approaches:
- Limit sugar and processed carbs. Read labels and avoid any beverages or foods that contain high-fructose corn syrup, agave, or other added sugars, as well as “no added sugar” fruit juices, which deliver high levels of fructose without the fruit’s fiber to mitigate its impact on blood sugar, says Harris. And avoid the highly concentrated processed carbohydrates found in packaged foods such as bread, crackers, and cereal.
- Consider glycemic response. To anticipate whether various foods will spike your blood sugar, consider their glycemic index (GI) and glycemic load (GL).
“These are tools to help manage diet and blood sugar, but they’re not the only tools we can use,” says Lockhart. “People have different blood-sugar responses to food, so we often have to look deeper.” (For more on these metrics and their limitations, see “Measuring Up” below.)
- Eat balanced meals. Whole-food nutrients including fiber, protein, and healthy fat mitigate blood-sugar spikes and subsequent insulin surges. And while phytonutrients in plant foods don’t slow the flow of insulin, they may help reduce some of the cellular damage that high levels of circulating blood sugar and insulin cause. So keep balance in mind as you prepare meals and snacks.
“Rice has a high glycemic index,” explains Harris, “but if you eat it with chicken (a protein) that has been cooked in olive oil (a healthy fat), and serve with artichokes and asparagus (fiber), the absorption of the rice is slowed and it won’t raise blood sugar as quickly.”
- Pay attention to your body. An analysis of how specific foods affect you begins with monitoring how your body responds to them. Do you feel irritable and shaky? Do you crave more food 30 to 40 minutes later? Are you fatigued? If so, your meal likely pushed your blood sugar and insulin beyond the healthy range.
Try a similar meal the next day but reduce the amount of sugar and carbohydrates, or increase the amount of healthy fat and fiber, and see if your response changes. When you find a combination of foods that allows you to go three to four hours before feeling hungry again, it’s a sign your blood-sugar response to that meal is slower and steadier.
Of course, people struggling with symptoms of metabolic diseases aren’t the only ones who benefit from paying closer attention to blood sugar and insulin response. Even folks without blood-sugar problems can benefit from steadier energy throughout the day, as well as all the benefits of a properly functioning metabolism.
“I encourage everyone to think about blood-sugar stability,” says Lockhart. “Focus on eating more blood-sugar-stabilizing foods, including protein, healthy fats, legumes, and nonstarchy veggies, which crowd out simple sugars and keep your health risks down.”
Measuring Up: Glycemic Index and Glycemic Load
If you’re trying to manage your blood sugar and insulin levels, you’ve likely heard about using the glycemic index and its sibling metric, glycemic load, to anticipate how certain foods may affect your body. This is how they work.
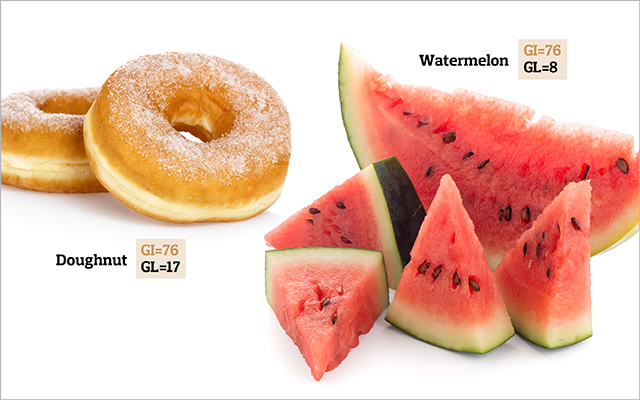
Glycemic index (GI) is a measure of a food’s potential to raise blood glucose relative to pure glucose, which has a glycemic index of 100. Foods that contain carbohydrates can be
classified as follows:
- GI of 70 or above: high
- GI of 56-69: medium
- GI of 55 or below: low
The glycemic index helps explain how some whole foods can cause big surges in blood sugar: Glucose is a prevalent carbohydrate in starchy vegetables such as potatoes (GI = 111). Meanwhile, nonstarchy vegetables have lower levels of blood-sugar-spiking carbs. Broccoli, for example, has a GI of less than 15 — and provides fiber and nutrients that help balance blood sugar and improve insulin response.
Because individual responses to glucose vary so widely, and glucose levels can change based on how food is prepared, the use of GI as a tool for managing blood sugar has become controversial.
Glycemic load (GL) goes a step further than GI by taking into consideration the amount of carbohydrate in a serving of a particular food. Most experts consider GL a better measure of a food’s impact on blood sugar.
To see how GL changes the evaluation of blood-sugar impact, consider the doughnut and the watermelon. The GI of these two is the same: 76. But when you look at the amount of carbohydrate in each, you learn that one serving of watermelon has 11 grams of carbohydrate due to its higher water content, while the doughnut has 23 grams.
To calculate GL, multiply the GI by the grams of carbohydrate in a serving, and then divide by 100.
Applying this formula reveals that the watermelon has a GL of 8, while the doughnut has a GL of 17.
- GL of 20 or above: high
- GL of 11-19: medium
- GL below 10: low
The Skinny on High-Sugar Diets
Blood-sugar and insulin problems are not an issue for just overweight and obese people. The ill effects of a high-sugar, high-carb diet can be borne by anyone. And it can catch people off-guard.
“People have the illusion of protection if they have a low body mass index,” says Aseem Malhotra, MD, coauthor of The Pioppi Diet. “But up to 40 percent of lean individuals have the same metabolic abnormalities as individuals with obesity.”
Indeed, almost one-third of Americans have prediabetes — and most of them don’t know it, according to a recent report from the Centers for Disease Control and Prevention. If not treated, prediabetes often leads to type 2 diabetes within five years.
This originally appeared as “Sugar Rush” in the May 2018 print issue of Experience Life.



This Post Has 0 Comments